Your Behavioral Health Ecosystem
With Lucet, optimize your health plan members’ access to behavioral health and achieve better outcomes at a lower cost.
We are the country’s leading behavioral health optimization company—removing complexity and providing the infrastructure for health plans and providers to optimize access to behavioral healthcare through quality, speed, and outcomes.
Introducing Navigate & Connect
Lucet’s tech-enabled solution combines a team of care navigators with an advanced technology platform built upon 20+ years of clinical research.
A Solution for Every Member
Health plans can clinically assess all members needing behavioral healthcare–from the mildest to the most complex–and direct them to care quickly.
Our Member Care Center enables:
- Proactive, targeted outreach to enroll & engage your members in need
- Screening members across the entire acuity spectrum
- Support with an extensive background in behavioral health and crisis management
- A positive impact on member experience

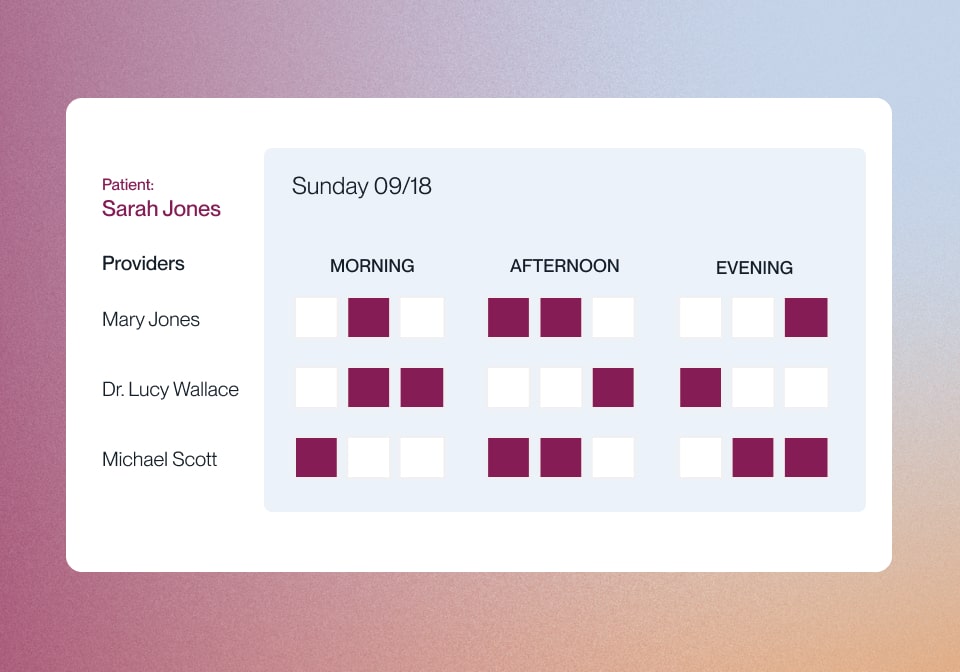
Appointment Scheduling at First Interaction
Lucet consolidates all network providers and point solutions on one technology platform. This access to pooled provider availability enables real-time appointment scheduling.
- Robust clinical screening process
- Supplemental network capacity
- Provider-friendly user experience
- Market-leading speed to care
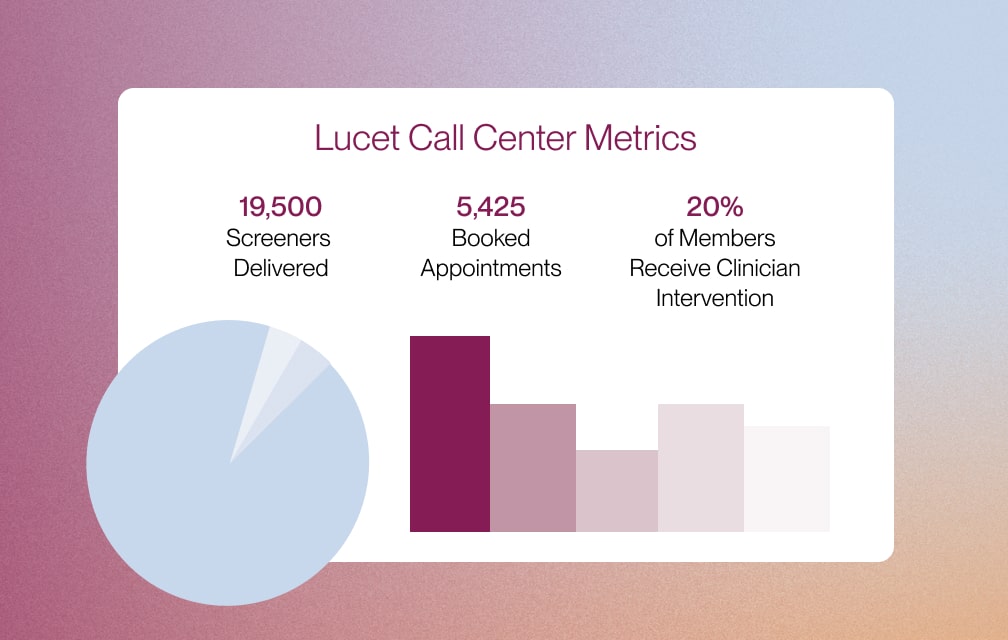
Comprehensive Insights Across the Ecosystem
Navigate & Connect delivers granular insights into member demand, network supply, performance, and clinical outcomes. We enable health plans to make real-time, data-driven decisions that can inform:
- Network management
- Sub-specialty needs analysis
- Value-based contracting
Dynamic Provider Network Management
Health plans working with Lucet’s Navigate & Connect technology have access to a new approach to provider network management that’s responsive to member demand.
- Analytics engine aligns member demand and provider capacity
- Dynamic provider stack management
- Comprehensive provider management services
Concierge-level Service for Your Members
Our clinically-informed care navigators and licensed clinicians provide behavioral health benefits, clinical management, and crisis intervention coverage across the clinical acuity spectrum.
- Identify and engage high-risk members
- Ongoing support and guidance for complex members
- White glove member services to get the right care for their needs
- 24-hour crisis support

How We Optimize Your Behavioral Health Ecosystem
Our Navigate & Connect Platform Offers:
Meet Lucet. We are the only company delivering real-time behavioral health optimization.
Learn MoreAdditional Behavioral Health Services
Lucet serves those who are affected by mental illness and impacted by trauma. We offer the most cost-effective care, from integrated care coordination to specialty clinical programs.